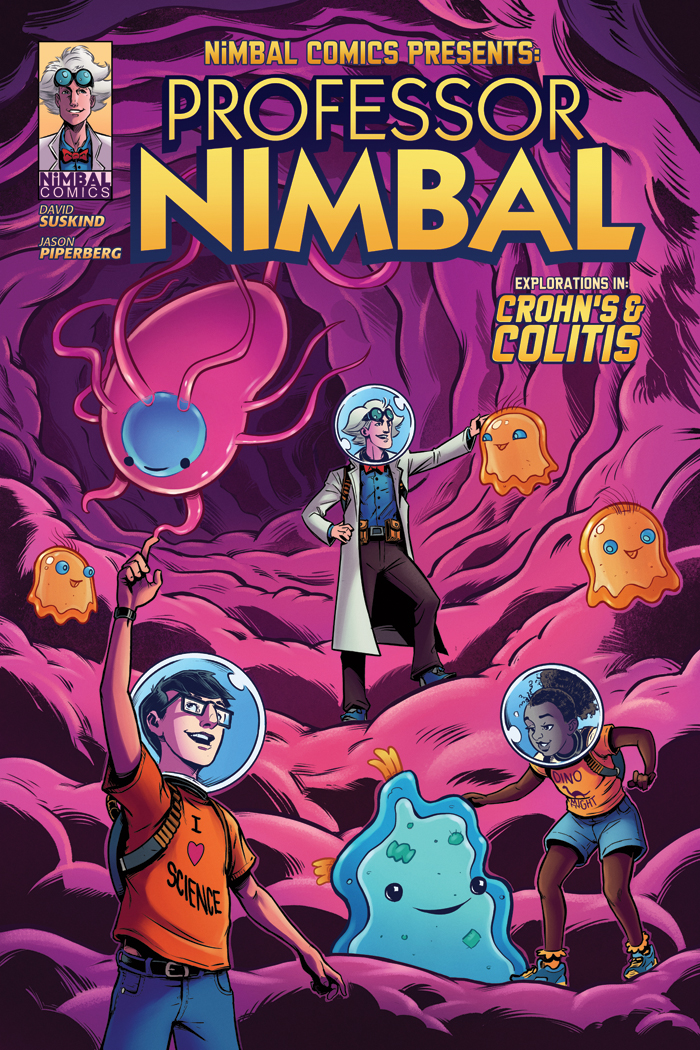
What are the types of inflammatory bowel disease?
Two main subtypes of IBD exist: Crohn’s disease and ulcerative colitis. Both are characterized by an attack on the bowels by the immune system, causing the harmful inflammation in IBD. The two subtypes differ in where the attack occurs, how the patient is affected, the way each progresses clinically and how the disease looks to the healthcare provider.
Crohn's disease
Text: In Crohn’s disease, inflammation can occur anywhere from the mouth to the anus. Inflammation can result in stricturing (narrowing of the bowels) or produce abscesses and fistulas, which are abnormal connections between the bowels and the skin, bowel, or organ. Crohn’s disease is usually described as being “patchy,” involving just one part or many parts of the bowels. Patients with Crohn’s disease can have a variety of symptoms. Symptoms are usually dependent upon what part of the bowels is affected and how much inflammation is present. Some patients may have recurrent oral ulcers which can make eating uncomfortable. If the stomach or duodenum (first part of the small intestines) is affected, you can have pain in your upper abdomen. The small intestine which is made up of three parts, the duodenum, jejunum, and ileum, is the longest part of the intestines but with the smallest diameter which is why it is called the ‘small' intestines. Its main job is to absorb nutrients. When the small intestines aren't working properly, you can develop significant abdominal pain along with nutritional deficiencies and weight loss. 2/3rds of people with Crohn’s disease have complications with their small intestines.
The colon is the end part of the intestines situated right before stool leaves the body. The reason it is called the large intestines is based upon its diameter which is larger than that of the small intestines. One of the colon’s function is to absorb excess water in the stool. When the colon gets irritated or inflamed, you can develop diarrhea and cramping with a bowel movement. If the rectum, the last part of the colon, gets irritated, it sends a message to the brain telling it that the body needs to go to the bathroom. Because of this, patients with irritated rectums will often complain about feeling the need to go the bathroom without any stool or just a small amount of stool coming out. This is called tenesmus. additionally, when the colon is affected, blood can sometimes leak into the stool so, colonic disease is characterized by bloody diarrhea. While medicines are effective in treating it, active Crohn’s disease also carries a high likelihood of the need for surgery within five years of diagnosis. This surgery will not, unfortunately, cure the patient of his or her Crohn’s.
Ulcerative colitis
In ulcerative colitis (UC), inflammation is present within the colon (large intestines) and is contiguous, meaning that it starts at the rectum and continues without any break ups through the colon. For some patients, only a small part of the colon is affected. If the inflammation is in the rectum, it is called “proctitis.” For others, the entire colon can be involved. This is called “pancolitis.” Symptoms of ulcerative colitis are the same as if someone had Crohn’s colitis with symptoms dependent on the degree and extent of disease. Unlike Crohn’s disease, if you have surgery to remove the colon to treat the UC, the disease can be cured.
Other IBD manifestations and factors
While we talk mostly about two types of IBD—Crohn’s and ulcerative colitis—in truth, the term represents many different types of bowel disease and each individual is unique in his or her presentation and response to medication. That said, there are commonalities for individuals with IBD and long-term observation has taught us a lot about the disease. Our ever-expanding technology gives us more tools to determine genetic and environmental influences on diseases and how they express themselves in each of us.
For example, we know that if you smoke and have Crohn’s, your disease is far more difficult to treat. If you are a smoker and have UC and you stop smoking, there is a higher likelihood that you will have a flare-up of your symptoms. (Of course, it is best to stop smoking to improve overall health.)
We also know that IBD is more common in the northern hemisphere than in the southern one. If you have the genetic abnormality NOD2, your disease is more likely to be in the ileum, the last section of the small intestine. Younger children usually present with more aggressive UC than their adult counterparts, and more often than not, pediatric UC affects the entire colon.
Most importantly, no matter how much we know about epidemiology and science, IBD is highly personal and specific to each individual. One person’s experience with ulcerative colitis or Crohn’s is not necessarily identical to another’s.
The more you know, the easier it will be.
A diagnosis of inflammatory bowel disease can be overwhelming. It can be a shock, and it can be depressing. But the first thing to say to yourself is, “We have a problem, we are going to handle it, and we are going to find a way to solve it the best way we can.” Being proactive, believe it or not, is halfway to a cure.
One of the most pressing questions you might have is: how exactly will this affect my life or my child’s life?
A good place to begin is with your healthcare provider. Ask the questions you need answers to (writing them down beforehand helps). If you need clarification on anything your provider shares with you, be clear about what information you need with questions like, “I really don’t understand what you’re saying,” or “Perhaps you didn’t really understand what I was asking you.” The more honest you can be, the clearer you are, the more likely you’ll get the answers you need.
Read—a lot. Find out from those who have gone through this before which books and resources they found most helpful. I would, however, caution you about the Internet. I have found more misleading than factual information online, and this sometimes leads newly diagnosed families to panic. Don’t panic—join support groups instead. Sometimes reassurance comes not just from what you hear in these groups, but from being with others who are going through the same experience—because while you’ll learn from them, they will also learn from you.
Over time, with the support of friends, family, your medical healthcare practitioner and others with inflammatory bowel disease, you will understand the disease, you will be able to help yourself and your child, and your child and you will live a healthy happy life, even while living with IBD.
The most important thing a parent can do is to give their child support, reassurance, guidance and love. And, when it is you who need help, reach out to those who can give you that same support, reassurance, guidance and love in turn. Supportive friends, family, and community can make all the difference. Make sure that your child receives the best healthcare available. Speak up when you have questions, especially when those questions come from the child who is learning about their disease. I’m a big fan of summer camps and the many wonderful programs for young adults and children with IBD, including those put on by the Crohn’s and Colitis Foundation of America (CCFA). These camp experiences help children understand and actually experience that they are not alone and that a like-minded community is there to support them. Knowing this is a great boost to the brain and self-esteem as well!